In Vitro Fertilization (IVF/ICSI)
In Vitro Fertilization (IVF/ICSI)
In vitro Fertilization (IVF) refers to the whole process by which eggs (oocytes) are stimulated to be mature, then retrieved from the ovaries, and joined with sperm, in vitro (in the laboratory), in order to obtain embryos that are later transferred inside the mother’s uterus to get a pregnancy.
When is it used?
IVF is currently the main treatment for infertility, and is indicated in many scenarios:
• Women with irreversibly damaged Fallopian tubes.
• Couples with multiple failures of other infertility treatments (ovulation induction, intrauterine insemination), regardless of the cause of infertility.
• Men with severely altered sperm parameters (moderate and severe male factor infertility).
• Couples with unexplained infertility of long duration (≥3 years).
• Women with endometriosis related infertility.
• Advanced maternal age.
• Couples needing a Preimplantation Genetic Diagnosis (to prevent the transmission of hereditary diseases).
What are the different steps of IVF ?
An IVF cycle requires approximately between 12 to 20 days from start to finish, and includes several steps:
• Controlled Ovarian Stimulation.
• Oocyte Retrieval (Egg collection)
• In vitro Fertilization with or without ICSI (Intracytoplasmic Sperm Injection).
• Embryo culture.
• Embryo transfer.
• Luteal phase and Pregnancy test.
• Cryopreservation of supernumerary embryos.
Frozen Embryo Transfer
Controlled Ovarian Stimulation
Controlled Ovarian Stimulation (COS) allows to obtain multiple mature oocytes (instead of one single oocyte that ovulates in a normal cycle), in order to increase the chances of pregnancy. It starts with an ultrasound performed on the first or second day of the menstrual cycle, in order to confirm the number of follicles and rule out any cysts. Daily subcutaneous injections of Gonadotropins are then started; these injections are patient friendly and can be performed by the woman or her partner at home, or by a nurse or the local pharmacist. The type and dose of gonadotropins, as well as the COS protocol, are chosen by the physician based on several elements (age, ovarian reserve…).
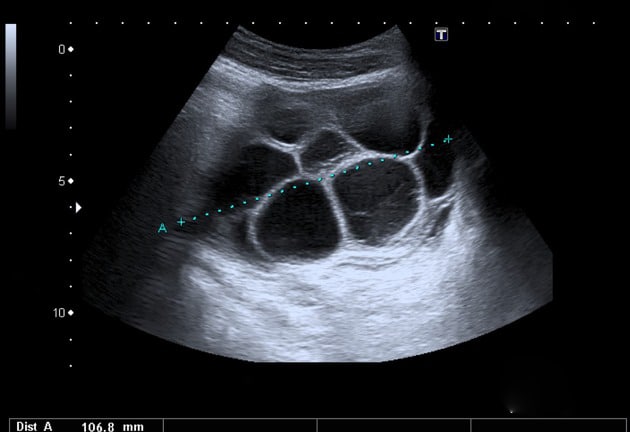
During COS, the patient needs several visits the doctor’s office (3-4 on average), where she undergoes a pelvic ultrasound and a blood test to monitor the response to stimulation (follicular growth and endometrial thickness). When the tests confirms that the follicles are ready (≥3 with a diameter ≥17-18 mm), an ovulation injection is prescribed (usually hCG), and the oocyte retrieval scheduled 36 hours later.
Oocyte Retrieval (egg collection)
The oocyte retrieval is the procedure that allows to recover the mature oocytes from the ovaries. It is performed in the operating theater of the IVF laboratory, and usually requires 15 to 20 minutes. It is usually performed under light sedation, so the patient should be fasting from midnight of the previous day. The retrieval is done through the vagina, under ultrasound guidance, using a specific needle to aspirate the fluid from all the follicles. The fluid is immediately passed to the laboratory to isolate the oocytes and prepare them for fertilization. After the retrieval, the patient rests in the recovery room for about an hour before being discharged home, and she can resume her everyday activity the following day. The partner gives the sperm on the day of the oocyte retrieval, following a period of abstinence of 2-5 days.
In vitro Fertilization with or without ICSI (Intracytoplasmic Sperm Injection)
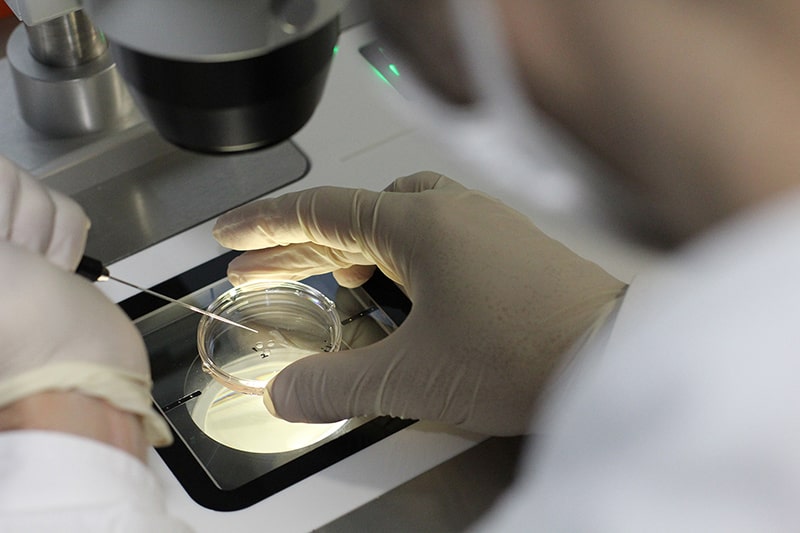
This step is the cornerstone of the cycle: In vitro (in the laboratory), the sperm fertilizes the mature oocyte, to produce an embryo. There are two techniques of in vitro fertilization: Conventional IVF, where the mature oocytes are placed in a culture plate with the sperm cells, allowing for natural fertilization to occur; and Intracytoplasmic Sperm Injection (ICSI), where each sperm cell is individually selected and microinjected inside each mature oocyte. The physician and the embryologist will take several factors into consideration (cause of infertility, quality of sperm…) when deciding which of these two techniques to use. On the following day, the fertilization is checked: each fertilized egg is now considered an embryo.
Embryo culture
Following fertilization, the embryos are placed in small dishes containing “culture media” to allow them to divide and develop normally. The dishes are placed in “incubators” that control the environment (temperature, atmospheric pressure…) and keep it suitable for the embryos to grow.
Embryos are kept in culture for a period of 3 to 6 days, during which they are periodically monitored by the embryologists. Several factors are taken into account when assessing the quality of an embryo: the number of cells, the fragmentation, the morphology, the speed of division… It is important to note that not all oocytes will be fertilized, and not all embryos will develop normally.
The best embryos will be chosen to be transferred and cryopreserved, while the poor quality embryos will stop developing and be discarded.


Embryo transfer
Embryos can be transferred back to the uterus on day 3, 5 or 6 after the retrieval. The main condition is that the endometrial lining (inner layer of the uterus) is adequate (thickness and appearance), which is confirmed by a pelvic ultrasound. The transfer is performed at the IVF laboratory as an outpatient procedure. It is painless, does not require any anesthesia, and takes approximately 10 minutes. With the patient lying in the supine position, a transfer catheter is gently inserted into the uterus, under ultrasound guidance. Once the catheter is confirmed to be in the right place inside the uterus, the embryos are loaded into the catheter and transferred into the uterus. The patient remains lying for 30 to 45 minutes after the transfer, and is discharged immediately after.
The decision on the number of embryos and the day of transfer is made by the treating physician and the embryologist, based on many clinical (age, history of previous treatments, type and duration of infertility) and biological (number and quality of embryos, endometrial thickness…) factors. Nowadays, the Gold standard is the transfer of a single blastocyst (Day 5 embryo) (Single embryo transfer). Indeed, extended culture to the blastocyst stage (Day 5) allows for the selection of the embryos with the highest implantation potential, and the transfer of a single embryo allows to reduce the risk for multiple pregnancies.
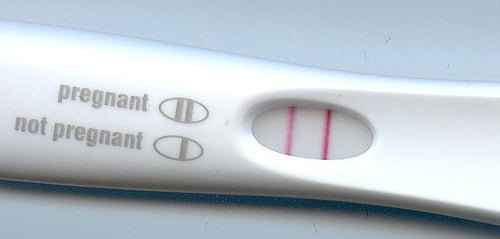
Luteal phase and Pregnancy test
The luteal phase refers to the period of time between the oocyte retrieval and the pregnancy test. It is a crucial period for the implantation of the embryo and the achievement of a healthy pregnancy. Progesterone is always added during the luteal phase to support the embryo implantation. Depending on the case, other medications could be added. The patient may resume normal daily activity during that period, although it is better to avoid high intensity activities.
The pregnancy test is usually performed 9 to 12 days after the embryo transfer. A blood test (quantitative bHCG measurement) should be performed, regardless of the patient’s symptoms. A positive test is usually repeated after 48 hours to confirm the evolution of the pregnancy. The patient with a positive test should contact her treating physician for future directives. The first ultrasound to confirm the pregnancy is usually performed two to three weeks after the positive test.

Cryopreservation of supernumerary embryos
For couples who have many good quality embryos, it is recommended to cryopreserve (freeze) the extra embryos that were not transferred. These extra embryos provide further opportunities for future pregnancies without going through the whole IVF process. Nowadays, embryos are cryopreserved by vitrification, an ultra-rapid freezing method, and stored in liquid nitrogen at -196 oC. Once frozen, the embryos can be stored indefinitely, without any alteration in their quality.
Frozen Embryo Transfer
Frozen embryo transfer (FET) is nowadays an integral part of infertility treatments. It allows couples to have multiple embryo transfers without the need for multiple ovarian stimulations and oocyte retrievals, thus increasing their chances of pregnancies, and their chances of having many babies. It is now well established that, in experienced centers, embryos frozen by vitrification offer the same pregnancy rates as fresh embryos. Moreover, the safety of embryo vitrification has now been confirmed, and there are no health risks for the babies born from vitrified embryos.
A FET can be programmed in a natural cycle, or using hormonal treatment (estrogen pills or patches), depending on the case. A visit is programmed at the beginning of the cycle, and another one to confirm if the endometrium is ready (thickness and appearance). The transfer, luteal phase and timing of the pregnancy test are highly comparable to fresh transfers.
Complications of IVF
IVF is associated with a relatively low rate of complications, most of them minor. The major complication of IVF is Ovarian Hyperstimulation Syndrome (OHSS). Here is the list of complications in each part of the IVF process:
Controlled Ovarian Stimulation
The Gonadotropins injected during COS can cause the following symptoms:
• Mild bruising or temporary allergic reaction at the subcutaneous injection site.
• Abdominal bloating and breast tenderness.
• Nausea and rarely vomiting.
• Fatigue and mood swings.
• Increased vaginal discharge.
In general, all these symptoms are minor and do not lead to discontinuation of the treatment. The patient should contact her treating physician if these symptoms appears.
Oocyte retrieval (Egg collection)
• Mild to moderate abdominal and pelvic pain, during the procedure or for a couple of days after. This is directly related to the retrieval, and can be managed with pain medication prescribed by the treating physician.
• Light vaginal bleeding (spotting) for a couple of days, directly related to the procedure.
• Injury to organs adjacent to the ovaries (Bladder, bowels, vessels…) that can lead to severe abdominal and pelvic pain, fever, and bleeding. This complication is very rare, and is usually diagnosed during the procedure.
• Pelvic infection, also very rare, causing fever and chills.
Embryo transfer
• Abdominal cramps, during or immediately after the transfer.
• Pelvic infection in extremely rare cases.
Luteal phase
The symptoms described in the COS phase can also be experienced during the luteal phase:
• Abdominal cramps and bloating.
• Breast tenderness.
• Fatigue and mood swings.
• Constipation.
• Ovarian torsion can occur in extremely rare cases and causes severe abdominal pain.
Early pregnancy complications
In general, pregnancies obtained by IVF are not considered at a higher risk than spontaneous pregnancies. The major complications in early pregnancy are:
• Pregnancy loss (miscarriage): The risk is the same as the general population, and depends on the patient’s age and medical history.
• Ectopic pregnancy: The risk is comparable to that in the infertile population, and depends on several factors (previous history of surgeries, infection…). Heterotopic pregnancy (One ectopic and intrauterine pregnancy) is a very rare complication of IVF occurring after the transfer of ≥2 embryos, and requires urgent management.
• Multiple pregnancies (twins, triplets…): The risk is higher than the general population, but depends on the number of embryos transferred. The Single Embryo Transfer on Day 5 policy significantly decreases the rate of multiple pregnancies.
Ovarian Hyperstimulation Syndrome (OHSS)
Ovarian Hyperstimulation Syndrome (OHSS) is an excessive response of the ovaries to controlled ovarian stimulation, and is the most serious complication associated with IVF. Women with OHSS have a high number of growing follicles, and high estrogen levels, causing significant fluid retention in the body. The risk factors of OHSS are young age, Polycystic Ovarian Syndrome, high ovarian reserve, low body weight, large number of growing follicles and high estradiol levels, high gonadotropin doses, and previous history of OHSS.
OHSS can be mild, moderate or severe:
• Mild to moderate OHSS: Symptoms include bloating, increased waist size, mild abdominal pain, nausea and vomiting, diarrhea, and weight gain.
• Severe OHSS: Severe abdominal pain, constant nausea and vomiting, rapid weight gain (≥ 1Kg/day), enlarged abdomen, shortness of breath, and decreased urination. In extreme cases, blood clots and kidney failure can be observed.
The treatment of OHSS depends on the severity. Mild to moderate OHSS can be treated in an outpatient setting, with a regular follow-up by ultrasounds and blood tests, fluid restriction, decreased activity, and symptomatic treatment. Severe OHSS calls for hospitalization for close monitoring and adequate treatment, and might require drainage of the excess fluid from the abdomen.
Nowadays, OHSS can be successfully prevented with the following measures:
• Careful screening of patients at risk.
• Prescribing individualized treatment plans.
• Using the antagonist protocol and the GnRH agonist trigger in women at risk.
• Freezing embryos and canceling the embryo transfer in women at risk.
The application of these preventive methods in the past decade has significantly decreased the risk of OHSS in IVF patients.
