Fertility Preservation (FP)
Fertility Preservation (FP)
Fertility preservation (FP) refers to the techniques that allow women to preserve their eggs (oocytes) and men to preserve their sperm cells for future pregnancies.
Egg Freezing (oocyte cryopreservation)
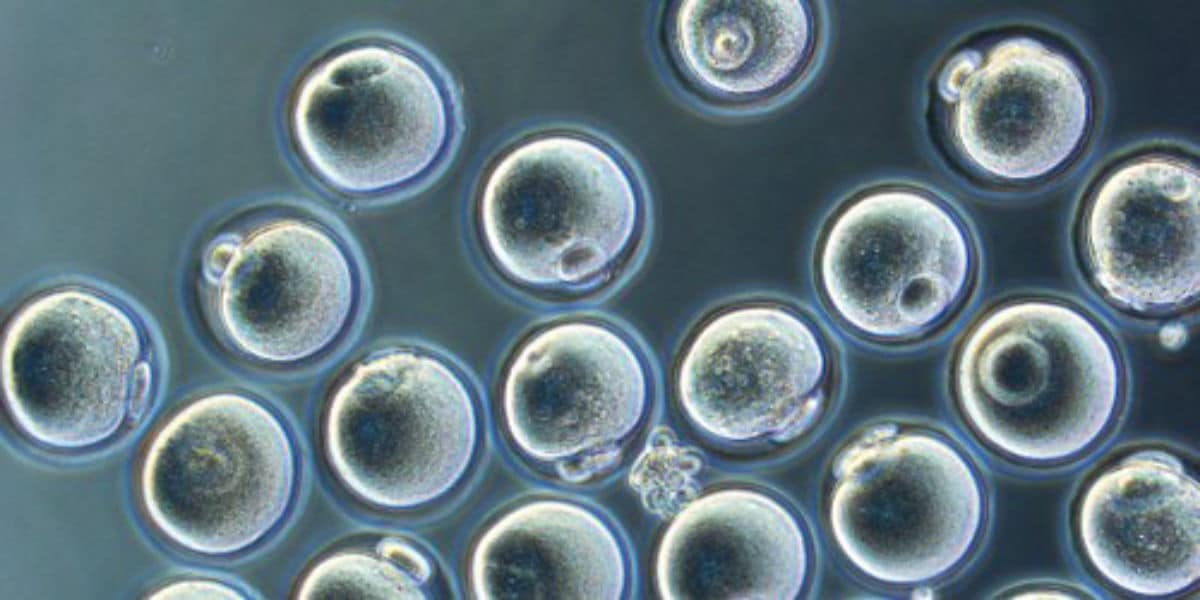
Egg freezing, or oocyte cryopreservation, allows women to postpone motherhood by cryopreserving their mature oocytes. Oocytes are frozen using vitrification, an ultra-rapid freezing method, and stored in liquid nitrogen at -196 oC.
Egg freezing is recommended in:
• Women at risk of losing their fertility because of an illness or a toxic treatment. This is referred to as “medical egg freezing”.
• Prevention of age-related fertility decline, also referred to as “social egg freezing”.

Oocyte cryopreservation for medical reasons – Medical egg freezing
The improvements in cancer treatments, and the efficiency of early screening programs, have significantly improved the survival rates. For instance, breast cancer, the most common cancer in women, has an overall survival rate ≥80%. Many cancer survivors are still young and want to start or expand their family. Unfortunately, cancer treatments are highly toxic, and can irreversibly damage a woman’s ovarian reserve, and her ability to conceive. Indeed, chemotherapy and pelvic radiation therapy significantly impair the ovarian reserve (Oocyte number and quality) and can lead to premature ovarian insufficiency (POI).
Therefore, it is now recommended that any woman of reproductive age diagnosed with cancer should be referred to a Reproductive Specialist, as soon as possible, before the start of treatment, to discuss the possibility of egg freezing. The procedure requires 1- to 14 days, and does not impact the condition nor delay the treatment. When the patient has successfully completed her treatment and it is safe for her to get pregnant, the oocytes are thawed, and fertilized with the partner’s sperm (using ICSI), and the resulting embryos are transferred back into the uterine cavity (see embryo transfer and frozen embryo transfer), without the need for a hormonal stimulation.
Besides cancer, any condition or treatment that could irreversibly impact the ovarian reserve is an indication for oocyte cryopreservation:
• Non-malignant chronic illnesses requiring toxic treatment, such as autoimmune diseases (severe systemic lupus, inflammatory bowel diseases…).
• Hematopoietic stem cell transplantation, for oncological and non-oncological illnesses. The protocols for stem cell transplantation include aggressive chemotherapy and radiotherapy, and are associated with a very high risk of ovarian insufficiency.
• Congenital conditions associated with premature ovarian insufficiency, such as Turner’s syndrome or fragile X-associated POI.
• Women with a positive family history of premature menopause.
Any surgery that may cause damage to the ovaries (endometriosis, ovarian cyst, pelvic surgery…) is also an indication for egg freezing.
Oocyte cryopreservation for prevention of age-related fertility decline – Social egg freezing
The ovarian reserve declines with age, and so does a woman’s fertility. Women’s peak fertility years extend from the early twenties till the early thirties, during which many of them are still single, or unable to start their family. Oocyte cryopreservation allows women to store their oocytes, at a healthy young age, and for an indefinite period of time. If infertility occurs later in life, because of the age related decline, or for other medical reasons, the frozen oocytes can be used to improve the chances of pregnancy.
There is no ideal age for women to undergo oocyte cryopreservation, since many factors are taken into consideration when opting for treatment, such as the ovarian reserve, the menstrual history, the personal medical and surgical history, the family medical history, marital status… The quantity and quality of the available oocytes decreases with age, therefore making social egg freezing more efficient at a younger age. The decision to undergo oocyte cryopreservation, and the ideal timing, should be discussed between the woman and her treating physician.
Oocyte cryopreservation has been proven to be efficient and safe, with thousands of healthy babies born following oocyte vitrification. The success rates vary according to the age of the woman at the time of freezing, and the number of oocytes frozen. Once frozen, the oocytes survive indefinitely, and without any alteration in their quality. A woman can undergo several cycles of oocyte freezing (egg banking) if the number of oocytes is deemed to be insufficient. Undergoing the procedure does not decrease a woman’s ovarian reserve or advance her menopause.
The Procedure
Oocyte cryopreservation involves the same initial steps as an IVF cycle up until the oocyte retrieval (Controlled Ovarian Stimulation and Oocyte Retrieval (Egg collection)). The process requires 10 to 14 days, during which the patient can proceed with her daily activities. After the retrieval, the oocytes are vitrified and stored in liquid nitrogen, and the patient is discharged home, to rest for the remainder of the day. The risks and complications are the same as for IVF (See complications of IVF). However, the risk of Ovarian Hyperstimulation Syndrome (OHSS) is extremely rare with oocyte cryopreservation, since there is no embryo transfer to perform.
The eggs are placed in special vials that are deposited in tanks containing liquid nitrogen. They are stored at -196 oC, at a temperature where there is no cellular activity, and thus are not affected by the length of storage. The eggs are kept until the patient decides to use them, and can be discarded at any time at her request.
Ovarian cortex cryopreservation – Ovarian tissue freezing
Ovarian tissue cryopreservation involves the removal of a part of the ovary, cryopreserving it, and implanting it back into the pelvis when needed. This technique has already led to the birth of hundreds of healthy babies worldwide, but is still considered experimental and is therefore reserved for special cases of infertility. The current indications are:
• Women of reproductive age with cancer who have to undergo urgent chemotherapy and thus cannot undergo controlled ovarian stimulation (COS) for oocyte cryopreservation, since it requires 10-14 days.
• Women of reproductive age undergoing highly toxic treatment with a very high risk of premature ovarian insufficiency.
• Pre pubertal girls. It is the only fertility preservation method applicable since they cannot undergo COS because of the immaturity of their reproductive axis.
The procedure
Ovarian tissue cryopreservation involves three steps:
1. Ovarian tissue harvesting: Usually performed by laparoscopy, under general anesthesia. One part or the entirety of the ovary is removed, depending on the case and the risk of ovarian insufficiency, and immediately transferred to the IVF laboratory. The procedure is usually performed as a day-surgery, and the patient can start her chemotherapy the day after.
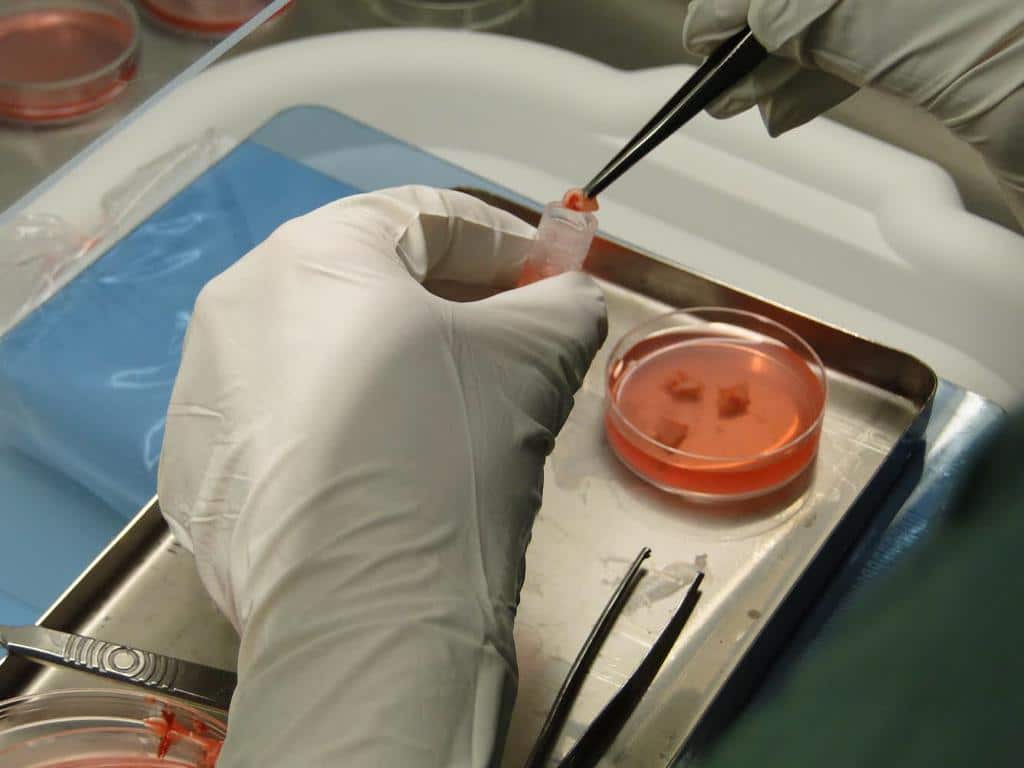
2. Ovarian tissue cryopreservation: In the IVF laboratory, the harvested tissue is placed in a special media, and the cortex is dissected away from the medulla and cut into small fragments to be cryopreserved. Only the cortex is preserved since it contains all the ovarian follicles that contain the oocytes. The fragments can be cryopreserved indefinitely without any alteration of the quality.
3. Ovarian tissue transplantation: Once the patient is disease-free and has the approval of her treating oncologist to get pregnant, and in case of ovarian insufficiency and infertility, the ovarian fragments are transplanted back into the pelvic cavity. The procedure is usually performed laparoscopically as a day-surgery. The implanted fragments resume their activity in the months following the procedure, and the patient can get pregnant spontaneously, or via IVF.
Sperm freezing – Sperm banking
Sperm freezing is the only proven method of fertility preservation in men and adolescents. Mature sperm cells are collected through masturbation and analyzed, before being cryopreserved via vitrification, and stored indefinitely in liquid nitrogen. In order to improve the chances of success, several samples can sometimes be required, especially in men with a decreased sperm count.
Sperm freezing has shown to be an efficient method of fertility preservation for more than 50 years, with millions of healthy babies born worldwide via sperm freezing. The safety of sperm freezing is also proven, and there is no risk on the health of the offspring. Frozen sperm can be used for an intrauterine insemination, an IVF cycle, or an ICSI cycle.
In patients and young adolescents having difficulty producing semen by masturbation, more invasive options, such as electroejaculation and testicular sperm extraction, can be proposed to allow sperm collection.
Sperm freezing is indicated in:
• Men diagnosed with cancer requiring chemotherapy or radiation therapy, since treatment has a direct negative impact on sperm cell production, an impact that can sometimes be irreversible. Sperm should be frozen before the start of chemotherapy, and does not delay the beginning of treatment, even when several samples are required.
• Men diagnosed with non-malignant chronic illnesses requiring toxic treatment, such as autoimmune diseases (severe systemic lupus, inflammatory bowel diseases…).
• Men requiring hematopoietic stem cell transplantation, for oncological and non-oncological illnesses. The protocols for stem cell transplantation include aggressive chemotherapy and radiotherapy, and are associated with a very high risk of testicular failure.
• Men with genetic ((Klinefelter’s syndrome…) or acquired disorders that may lead to progressive degradation of sperm production, and even azoospermia (Absence of sperm cells).
• Men undergoing testicular surgery that may irreversibly alter sperm production, for benign or malignant conditions.
• Men considering delayed parenthood and men with advancing age, since advanced paternal age has been shown to impact sperm production and the health of the offspring.
Men spending most of their time away from their partners while trying to conceive. In these instances, the chances of natural conception are decreased, and sperm freezing allows to perform Intrauterine Inseminations or IVF/ICSI cycles even when the man is abroad.


To date, fertility preservation in prepubertal boys remains challenging, because active spermatogenesis does not start before puberty. Therefore, prepubertal boys cannot benefit from sperm banking. There are several experimental procedures that are offered nowadays, such as immature testicular tissue, or spermatogonial stem cells cryopreservation. However, these techniques are still under investigation, for efficiency and safety, with many uncertainties about genetic and epigenetic consequences for the offspring., and are only offered as part of a research protocol.
